No one could offer anything but our deepest and most heartfelt thanks and a feeling of pride in the selfless, essential and humanitarian work being done by healthcare workers (HCWs), both local and international, in West Africa.
But they have paid a high price for this work, as they always do in emerging disease outbreaks.
Of the >5,300 people reported as infected by the West African variant of Zaire ebolavirus (EBOV) to date, around 315 have been HCWs. Both numbers are very likely an underestimate. Half of the HCW cases have died. I don't know just how many HCWs there are in Guinea, Liberia and Sierra Leone who are dealing with the EBOV outbreak. I do know that these deaths are as horrible as each of the losses among non-HCWs, and are also worrying for those trying to recruit the many more HCWs needed to expandthe care of ill patients.
This week a commentary article on the Centre for Infectious Disease Research and Policy (CIDRAP) website delves into this issue by suggesting an improvement to HCW respiratory protection.[1]
Two quick things first:
Some collaborators and I wrote about Ebola virus not being an airborne virus based on what I know and what's been done to answer this question before.[2] I'll first add that if it were an airborne virus, I would likely be seeing many, many more cases-"Compared to this Ebola outbreak, the H1N1 swine flu had already spread to an estimated 10,000 times as many people in its first 10 months" noted United Kingdom virologist Ben Neuman.[13] H1N1 being an influenza A virus; a real airborne virus. In our post, we noted that big wet droplets (part of an "aerosol"-a messy term that may not be well understood by the public...or some scientists...that includes big wet droplets and the more frequent smaller particles <100µM in diameter) can be propelled at a mucous membrane or fall to the ground to contaminate surfaces.
Big wet, propelled droplets can contain infectious Ebola virus and are included in the established risk messaging. Hence the need for droplet precautions.
We also know that from every human aerosol, after the heavy larger droplets fall to the ground or impact on a surface, the many more remaining lighter particles can linger in the air. I know that these small <100µm particles can be made to contain infectious Ebola virus under lab conditions[8] thus droplet nuclei produced by an infected human may contain Ebola virus. I can't say with certainty that they do or do not. However, as far as I have been able to tell, infection of humans and resultant disease from inhaling lingering particles, has not occurred. And when an airborne route was investigated using infected and uninfected non-human primates housed nearby but without direct contact, no infection via an airborne route was found to have taken place.[9]
Most of the studies looking at aerosols of Ebola virus do so in highly temperature and humidity-controlled laboratories with lots of lab-grown virus.
Relying on one added component raises a few questions for us:
The authors overlooked mentioning that early on, many HCWs may have had few or no masks at all and few other essential barriers such as those listed by WHO above, to protect against direct contact. They also did not mention the lack of HCW training in the use of any of that equipment if available, and did not highlight the lack of experience HCWs had dealing with EVD patients. These HCWs had (and may well still have) direct contact with very ill EVD cases, and got infected. What fraction of HCW infections resulted from absent or incomplete PPE and training versus the HCWs that they believe became ill while wearing full droplet precaution PPE?
Others have also made note of the disparities between the imagery of a biosafety level 4 (BSL4) laboratory researcher working in a negatively pressurized, airlocked laboratory within a tethered, airtight suit (probably unnecessarily high precautions [13]) versus highly biocontained single patients being shipped home on dedicated planes (kept somewhat contamination-free using isolators) to rich nations for specialized support and treatment versus Médecins Sans Frontières (MSF) workers who use respirators (specialized face masks that fit more snugly and contain more layers to better filter what is breathed in) instead of surgical masks versus the WHO recommendations of standard precautions which include a surgical mask. Notably, the WHO recommendations vary according to the type of risk one is exposed to [see pg 96-7 96 of the 113 pg PDF at [3]).[10] There clearly is a range of thinking and messages here. But equally, there are a lot of different applications to cover, and no way for every need to be specifically catered for by one guideline. If everyone could agree on such a thing anyway.
I share the concern of many over the deaths of HCWs in West Africa. They may still be unnecessarily exposed to the virus due to the lack of enough PPE. They may not have enough training to understand how easy it is to become infected. They may not be given the message that during an EVD outbreak as monstrous and different as this one, many heavily populated areas have been included for the first time resulting in very real risks of infection occurring outside the hospital setting, not just inside it. There are also real risks of infection in supposedly EVD-free hospital settings like maternity wards.[11] There are many, many non-airborne related risks for HCWs.
We freely admit that we are not trained in the use of PPE for treating Ebola patients; just for working with actual respiratory and blood-borne viruses in PC2 & PC3 laboratory settings, respectively. Still, some may find this post irrelevant.
But for what it's worth, I would follow the MSF lead if working on the battlefield of a 100+ bed treatment facility. In an ideal world, more effort would be made to provide a more roomy and breezy head covering that allows patients to see your face and which can be worn for longer periods would be useful. You can see an image provided by 3M of this battery-powered air-purifying respirator (PAPR) accompanying the CIDRAP post.
However....first and foremost, and well before we get to this level of hair-splitting based on speculation and belief and no evidence of an airborne virus-I'd be wanting to make sure there was a minimum level of disposable PPE actually available for use, that it was consistently used by every HCW, that appropriate training in its use had been provided, and that HCWs understood about all the risks for acquiring EBOV infection.
Reasons for HCW infections are many and varied. As much as we may believe or wish it were so, no single act or change will circumvent these risks or these infections.
References..
But they have paid a high price for this work, as they always do in emerging disease outbreaks.
 |
| WHO Ebola virus disease numbers up to 14-Sept-2014 |
This week a commentary article on the Centre for Infectious Disease Research and Policy (CIDRAP) website delves into this issue by suggesting an improvement to HCW respiratory protection.[1]
Two quick things first:
- The World Health Organization (WHO) defines human transmission of Ebola virus as being by direct contact (between mucous membranes or a break in the skin and the blood and other body fluids of an infected individual via physical contact or by wet material being propelling onto mucous membranes or skin breaks) and by indirect contact via contaminated surfaces.[3,4]
- When dealing with patients, the WHO recommends wearing gloves, a disposable impermeable gown to cover exposed skin, a waterproof apron over any gown that is not impermeable or when undertaking strenuous activity, facial protection to prevent splashes to the nose, mouth and eyes including a medical mask + eye protection (visor or goggles) or a face shield and medical mask.[3]
Some collaborators and I wrote about Ebola virus not being an airborne virus based on what I know and what's been done to answer this question before.[2] I'll first add that if it were an airborne virus, I would likely be seeing many, many more cases-"Compared to this Ebola outbreak, the H1N1 swine flu had already spread to an estimated 10,000 times as many people in its first 10 months" noted United Kingdom virologist Ben Neuman.[13] H1N1 being an influenza A virus; a real airborne virus. In our post, we noted that big wet droplets (part of an "aerosol"-a messy term that may not be well understood by the public...or some scientists...that includes big wet droplets and the more frequent smaller particles <100µM in diameter) can be propelled at a mucous membrane or fall to the ground to contaminate surfaces.
 |
| A schematic of the makeup of an "aerosol". From [2] |
We also know that from every human aerosol, after the heavy larger droplets fall to the ground or impact on a surface, the many more remaining lighter particles can linger in the air. I know that these small <100µm particles can be made to contain infectious Ebola virus under lab conditions[8] thus droplet nuclei produced by an infected human may contain Ebola virus. I can't say with certainty that they do or do not. However, as far as I have been able to tell, infection of humans and resultant disease from inhaling lingering particles, has not occurred. And when an airborne route was investigated using infected and uninfected non-human primates housed nearby but without direct contact, no infection via an airborne route was found to have taken place.[9]
Most of the studies looking at aerosols of Ebola virus do so in highly temperature and humidity-controlled laboratories with lots of lab-grown virus.
Relying on one added component raises a few questions for us:
- Could the faith in this one extra precaution threaten the very important, meticulous care required when donning, using, and removing contaminated PPE-of any sort?
- What role does a lack of the basics, like soap and clean water [10], play in HCW infections?
- Could an additional extra safety measure really have a major effect on reducing the known risks involved with treating Ebola virus disease (EVD) patients, such as the long hours, tiredness, the constant and pervasive tension of imminent exposure, the oppressive heat, delirious and sometimes violent patients and the ease with which one can self-inoculate?[6]
- Does the extra safety measure even have a role in reducing risk associated with HCWs who are unknowingly infected while not wearing PPE?[7]
The authors overlooked mentioning that early on, many HCWs may have had few or no masks at all and few other essential barriers such as those listed by WHO above, to protect against direct contact. They also did not mention the lack of HCW training in the use of any of that equipment if available, and did not highlight the lack of experience HCWs had dealing with EVD patients. These HCWs had (and may well still have) direct contact with very ill EVD cases, and got infected. What fraction of HCW infections resulted from absent or incomplete PPE and training versus the HCWs that they believe became ill while wearing full droplet precaution PPE?
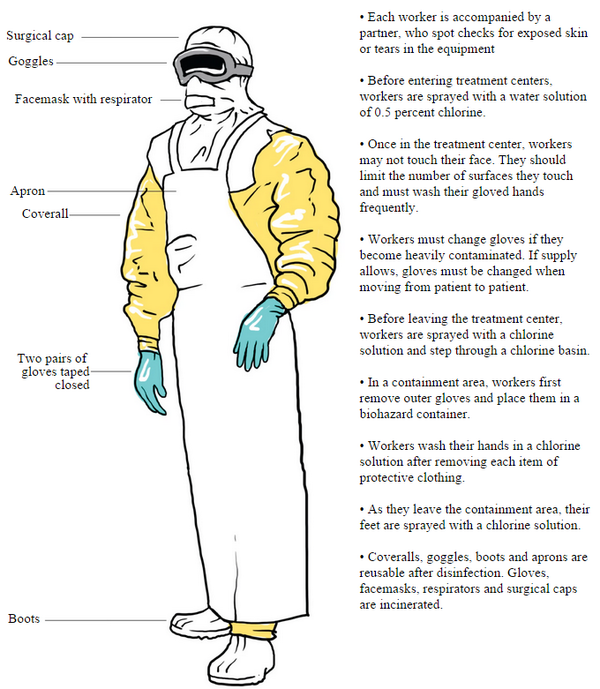 |
| MSF designed suit of PPE. Graphic tweeted by the Washington Post.[5] |
I share the concern of many over the deaths of HCWs in West Africa. They may still be unnecessarily exposed to the virus due to the lack of enough PPE. They may not have enough training to understand how easy it is to become infected. They may not be given the message that during an EVD outbreak as monstrous and different as this one, many heavily populated areas have been included for the first time resulting in very real risks of infection occurring outside the hospital setting, not just inside it. There are also real risks of infection in supposedly EVD-free hospital settings like maternity wards.[11] There are many, many non-airborne related risks for HCWs.
We freely admit that we are not trained in the use of PPE for treating Ebola patients; just for working with actual respiratory and blood-borne viruses in PC2 & PC3 laboratory settings, respectively. Still, some may find this post irrelevant.
Deeply concerned about bloggers with no PPE research track rec, no clinical or infection control expertise making recommendations about PPE.
— Raina MacIntyre (@RainaMacIntyre) September 16, 2014
This is a blog and not part of any Organization's reference list when they write PPE guidelines...because it's a blog.But for what it's worth, I would follow the MSF lead if working on the battlefield of a 100+ bed treatment facility. In an ideal world, more effort would be made to provide a more roomy and breezy head covering that allows patients to see your face and which can be worn for longer periods would be useful. You can see an image provided by 3M of this battery-powered air-purifying respirator (PAPR) accompanying the CIDRAP post.
However....first and foremost, and well before we get to this level of hair-splitting based on speculation and belief and no evidence of an airborne virus-I'd be wanting to make sure there was a minimum level of disposable PPE actually available for use, that it was consistently used by every HCW, that appropriate training in its use had been provided, and that HCWs understood about all the risks for acquiring EBOV infection.
Reasons for HCW infections are many and varied. As much as we may believe or wish it were so, no single act or change will circumvent these risks or these infections.
References..
- http://www.cidrap.umn.edu/news-perspective/2014/09/commentary-health-workers-need-optimal-respiratory-protection-ebola
- http://virologydownunder.blogspot.com.au/2014/08/ebola-virus-may-be-spread-by-droplets.html
- http://apps.who.int/iris/bitstream/10665/130883/2/WHO_HSE_PED_AIP_14.05.pdf?ua=1
- http://www.who.int/mediacentre/factsheets/fs103/en/
- http://apps.washingtonpost.com/g/page/national/suiting-up-for-ebola/1312/?Post+generic=%3Ftid%3Dsm_twitter_washingtonpost
- http://www.theguardian.com/world/2014/sep/21/ebola-makes-you-a-risk-to-yourself-sierra-leone
- http://www.nbcnews.com/storyline/ebola-virus-outbreak/are-hospitals-part-ebola-problem-charity-wants-new-strategy-n202486
- http://www.ncbi.nlm.nih.gov/pubmed/20553340
- http://virologydownunder.blogspot.com.au/2014/08/ebola-pigs-primates-and-people.html
- http://apps.who.int/iris/bitstream/10665/130596/1/WHO_HIS_SDS_2014.4_eng.pdf?ua=1&ua=1&ua=1
- http://abcnews.go.com/Health/latest-american-ebola-patient-headed-nebraska-hospital-treatment/story?id=25252017
- http://uk.reuters.com/article/2014/09/19/us-health-ebola-mutations-idUKKBN0HE0O320140919
- http://jid.oxfordjournals.org/content/179/Supplement_1/S287.full
Updates..
- 03092022-revised some excitable wording and clarified text around droplets and droplet nuclei to reflect the more recent understanding
No comments:
Post a Comment
Note: only a member of this blog may post a comment.